Why Fatigue Is So Hard to Solve
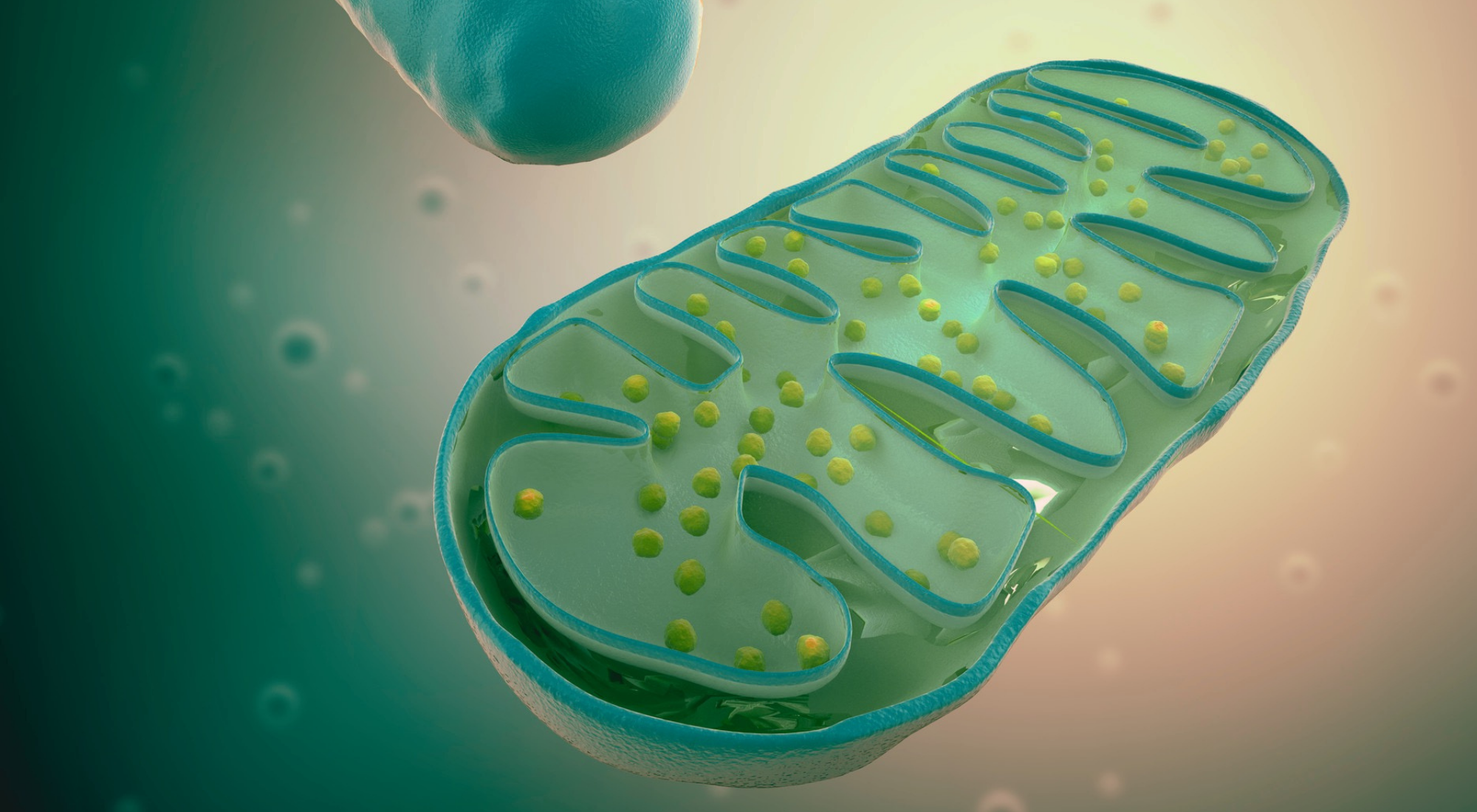
Mitochondria and fatigue are closely connected. If your mitochondria, the tiny power plants inside your cells, don’t work properly, no amount of sleep will restore your energy.
Fatigue is one of the most frequent and frustrating conditions I treat in my functional medicine practice. Yet it remains deeply misunderstood—not only in conventional medicine, but also in functional and precision medicine circles.
Why is fatigue so difficult to solve? Because it rarely comes from a single cause. Instead, it’s like peeling back an onion: once you address one layer, another issue appears beneath it.
Some common contributors include:
- Intestinal permeability (leaky gut)
- Thyroid disease
- Nutrient deficiencies
- Hormonal imbalances
- Mood disorders
However, one factor that gets far less attention is mitochondrial dysfunction.
Crash Course: What Are Mitochondria?
Mitochondria act like your body’s power stations. They turn oxygen and nutrients into ATP (adenosine triphosphate), the energy your body runs on. Without ATP, your organs and systems cannot function.
In addition, mitochondria regulate:
- Insulin secretion → stabilizing blood sugar
- Neurotransmitter synthesis → supporting mood and brain health
- CoQ10 and enzyme production → fueling metabolism
- Calcium balance → coordinating nerves and muscles
- Heat production → maintaining body temperature
Mitochondrial Dysfunction vs. Mitochondrial Disease
It’s important to clarify a distinction:
- Mitochondrial Diseases → rare, inherited disorders caused by mutations in mitochondrial DNA, usually diagnosed in childhood.
- Mitochondrial Dysfunction → far more common and acquired later in life, often linked to stress, toxins, inflammation, poor nutrition, or aging.
In this article, we’ll focus on mitochondrial dysfunction since it explains much of the fatigue seen in otherwise “healthy” adults.
How Inflammation Damages Mitochondria and Energy
Chronic inflammation drives disease, and it directly interferes with mitochondria:
- Inflammation increases energy demands on your immune system.
- Immune cells switch to a faster but less efficient energy process called aerobic glycolysis.
- This shift drains nutrient reserves and produces fewer ATP molecules.
- Oxidative stress builds, further damaging mitochondria.
As a result, even if you eat a nutrient-rich diet, your mitochondria may still struggle. In my clinic, I often see patients deficient in CoQ10, riboflavin (B2), niacin (B3), l-carnitine, lipoic acid, and vitamin E.
Read more at the NIH: Chronic inflammation and fatigue.
CoQ10: The Mitochondrial Antioxidant Superhero
Among mitochondrial nutrients, CoQ10 stands out. It:
- Acts as a cofactor in the electron transport chain for ATP production
- Protects mitochondria from free radicals
- Declines naturally with age, stress, chronic illness, and medications like statins
Low CoQ10 is linked with thyroid disorders, fibromyalgia, diabetes, cancer, and cardiovascular disease. Fortunately, supplementation can restore reserves and improve fatigue. See research on CoQ10 and energy.
The Mitochondria–Metabolic Health Connection
Fatigue often goes hand in hand with blood sugar imbalance. Mitochondrial dysfunction contributes to:
- Type 2 diabetes by impairing insulin release
- Insulin resistance by disrupting muscle signaling
- Mitochondrial diabetes, often mistaken for Type 1 or Type 2
In practice, a normal fasting glucose doesn’t always rule out issues. HbA1c and continuous glucose monitoring (CGM) give better insight.
How to Support Mitochondria and Restore Energy
Lifestyle Strategies
- Intermittent fasting → slows mitochondrial aging and balances blood sugar
- High-intensity interval training (HIIT) → increases mitochondrial number and insulin sensitivity
- Stress management → prevents inflammation-related damage
- Cold exposure → stimulates creation of new mitochondria
Nutrition
- Eat an anti-inflammatory diet: vegetables, fruits, omega-3s, grass-fed proteins
- Avoid processed foods, refined sugars, and inflammatory oils
Key Supplements
- CoQ10 → powers mitochondria and protects against free radicals
- Lipoic acid → reduces oxidative stress and improves blood sugar control
- L-carnitine → carries fatty acids into mitochondria for energy
- Nicotinamide riboside (B3) → supports mitochondrial biogenesis
- NAC (n-acetylcysteine) → replenishes glutathione, protecting mitochondria
- Resveratrol & Curcumin → reduce inflammation and enhance ATP production
FAQs: Mitochondria, Fatigue, and Functional Medicine
- What are the symptoms of mitochondrial dysfunction fatigue?
- Persistent tiredness, brain fog, muscle weakness, slow recovery, and nutrient deficiencies.
- Can supplements help mitochondrial fatigue?
- Yes. Studies support CoQ10, lipoic acid, l-carnitine, and NAC for improving mitochondrial health and energy.
- How do you test mitochondrial health?
- Functional medicine practitioners use nutrient panels, organic acid testing, HbA1c, inflammatory markers, and advanced metabolic assessments.
- Can mitochondrial dysfunction be reversed?
- In many cases, yes. With nutrition, lifestyle shifts, and targeted supplements, mitochondrial function and energy can improve.
- Why see a functional medicine doctor for fatigue?
- Because fatigue usually has multiple causes. Functional medicine uncovers root issues such as thyroid imbalance, gut health problems, blood sugar dysfunction, and mitochondrial fatigue.
The Bottom Line: Energy Begins in Your Mitochondria
If you’re constantly tired—even after 8 hours of sleep—your mitochondria may be the root cause. The good news? You can support mitochondrial function through anti-inflammatory nutrition, proven supplements like CoQ10, and functional medicine strategies.
If you’re in Texas, I’d love to work with you at Nourish Medicine. Outside Texas, visit the Institute for Functional Medicine Practitioner Finder to locate a certified provider.
For a step-by-step healing plan, check out my book Bloom, where I explain how to restore energy, balance your hormones, and reignite your spark.

Leave a comment